Short Communication 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Comparison of Diagnostic Significance of High Resolution Photocounting Computed Tomography (PHRCT) and Magnet Resonance Imaging (MRI) in Systemic Sclerosis Interstitial Lung Disease (SSC-ILD) - A Prospective Blinded Non-Interventional Mono- Centre Study of 20 Cases
*Corresponding author: Assmann Gunter Prof., MD, Department of rheumatology, RUB University Hospital Minden JWK, Minden, Jose Carreras Center for Immungenetics und Gene Therapy, University of Saarland, Homburg, Germany.
Received: June 19, 2024; Published: July 01, 2024
DOI: 10.34297/AJBSR.2024.23.003045
Abstract
Background: Lung involvement with ILD is extremely relevant for the prognosis for Systemic Sclerosis (SSc). In addition to pulmonary function testing including the determination of diffusion capacity, lung imaging is the decisive diagnostic tool for determining the indication for treatment and the course of the disease. High Resolution Photocounting Computed Tomography (pHRCT) is the established standard of imaging in SSc-ILD, Magnet Resonance Imaging (MRI) is an alternative tool, but with reduced informative value, however with optimal radiation hygiene.
Patients and Methods: We conducted a prospective blinded controlled study of 20 SSc-ILD cases at the RUB University Hospital Minden, Germany, to compare the findings of pHRCT and MRI of the lung. All patients underwent HRCT and MRI of the lungs (maximum 3 days apart), pHRCT was performed by high-resolution photoncounting HRCT (Siemens Naeotom, Siemens Healthcare, Erlangen); MRI use 3D Ultrashort-Echo-Time (UTE) MR sequence technique in free breathing in 0.55 Tesla low-field MRI (Magnetom Free.Max, Siemens Healthcare, Erlangen, Germany). All HRCT images were evaluated by three radiologists with high expertise in ILD diagnostics without knowledge of the respective MRI images and vice versa. The evaluation matrix comprised four uniform gradings of 1) interstitial fibrosis, 2) alveolitis/ground glass opacities, 3) pleural thickening and 4) the percentage manifestation of ILD in general. The correlation (according to Pearson and Spearman) between the HRCT and MRI findings (n=60, respectively) was determined using SPSS, a p-value<0.05 was assessed as significant. The interrater-investigator variability (between the three radiologists) was evaluated according to Fleiss kappa modality.
Results: The evaluations showed a relatively high agreement in the categories interstitial fibrosis degree (Pearson correlation 0.829) and gradual expression of ILD quantitatively (0.753), lower for alveolitis and pleural thickening (Figure 1). The results in all four categories had in common that the MRI mostly underestimated the severity due to the evaluation matrix. The interrater variability was significantly higher in MRI than in pHRCT (Fleiss kappa for MRI 0.05-0.256 vs. pHRCT 0.306-0.527).
Conclusion: The study shows acceptable correlation of the HRCT findings with the MRI findings, particularly with regard to the degree of fibrosis in SSc-ILD, although the MRI findings have been significantly underestimated and with higher interrater variability in comparison with HRCT. In our opinion, it is essential to specify the evaluation software for MRI optimizing the imaging of the special features of the lung parenchyma; further prospective studies to improve the MRI modalities are recommended before a broader use of MRI in SSc-ILD might be proposed.
Introduction
Systemic sclerosis is a rare autoimmune-triggered disease in which immune-mediated vasculopathy, inflammation and fibrosis of affected organs lead to their progressive loss of function [1]. The lung is a frequently affected organ that develops interstitial lung disease as a typical manifestation, which is associated with a poor prognosis. SSc-ILD can occur early in the course of SSc and is often initially asymptomatic. Screening SSc patients for ILD is therefore of great importance [2]. In addition to lung function testing, diagnostic imaging with CT is essential for the assessment of lung manifestations. Alternative imaging procedures such as sonography or MRI have not yet been able to establish themselves. However, especially in view of the radiation exposure, the use of MRI for the diagnosis and follow-up of various lung diseases is the subject of ongoning research. The technical modification of the MRI procedure plays an important role here in order to be able to optimally detect lung processes such as tumours or infiltrates without being able to reliably achieve the imaging quality of CT so far. However, technical developments in both CT and MRI imaging are increasingly changing this assessment: The lastest milestone in CT technology was the development and the introduction of the first photon counting CT (pHRCT, Naeotom Alpha, Siemens Healthineers, Erlangen, Germany) for clinical use in 2021, and for the MRI the Ultra-low-field magnetic resonance imaging for lung examinations applying VIBE sequence is a radio-frequency-spoiled 3D Gradient Echo (GRE) sequence untilizied in MRI to generate T1-weigthed three-dimentionsal images employing interpolation and/or partial Fourier techniques [3,4]. For SSc-ILD, there are no comparative studies on the use of pHRCT and MRI to date, which is why we present a non-interventional prospective blinded mono-centre study here. In the analysis, various typical pulmonary manifestations of SSc-ILD were taken into account, as well as the interrater variability of radiologists’ findings on pHRCT and MRI of the lungs of SSc-ILD patients.
Materials and Methods
Patient Population
This prospective single-center patient study was conducted according tho the Declaration of Helsinki and approved by the institutional review board (BOE/EK 2022). Only patients diagnosed with interstitial lung disease by systemic fibrosis were included as study participants, if they were older than 18 years and eligible for MRI examinations. All patients fulfilled the classification criteria of SSc according to the latest ACR/EULAR recommendation as previously published [5]. ILD was diagnosed in all cases in the conference of an ILD board together with radiologists, rheumatologists and pulmonologists. All pHRCT exams of the lung were performed for diagnostic use with clinical standard protocols. Informed written consent was given by all study participants in advance of ultra-low field MRI scans of the lung which were addintionally performed to pHRCT for scientific use only. Patient data were anonymized.
In total, 20 SSc-ILD patients (8 male, 12 female, Table 1) underwent low dose high resolution chest pHRCT between January and November 2023 in the clinical routine. At the same day or within the next three days all included patients unterwent a low field MRI examination of the lung performed with a 0.55 Tesla MRI scanner (MAGNETOM Free.Max, Siemens Healthineers, Erlangen, Germany) equipped with a contour M-body coil.
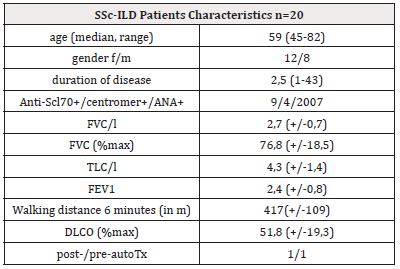
Table 1: characteristics of patients with Systemic Sclerosis (SSc) with Interstitial Lung Disease (ILD) underwent high resolution Computed Tomography (CT) and Magnet Resonance Imaging (MRI) according to study study protocol.
Note*: Anti-Sc70+=positive for anti-scleroderma autoantibody 70; centromere=positive for anti-centromer-autoantibody; ANA+=positive for auto-anti-nuclear antibodies (without SSc70 or centromere); FVC=forced vital capacity; TLC=total lung capacity; FEV=forced expiration capacity; DLCO=diffusion lung capacity of oxygen; post-/pre-autoTx=after/prior to autologous hemopoietic stem-cell transplantation.
pHRCT Protocols and Image Acquisition
All study participants underwent non-enhanced LD-HR CT scans of the chest with the pHRCT and software version Syngo CT VA 40, Siemens Healthineers, Erlangen, Germany. All CT examinations were performed in supine position. The scan parameters of the pHRCT were as follows: tube voltage=120 kVp, detector configuration=144 x 0.4 mm, automatic tube current modulation, image quality (IQ-level) =70, pitch=1.2 and gantry rotation time=25 s. The reconstructed images were analyzed retrospectively using a standard PACS system (IMPAX 6.7, Agfa Healthcare, Mortsel, Belgium). All images were reconstructed in axial and coronal view with the same slice thickness (1mm). The pHRCT images were reconstructed with quantum iterative reconstruction (QIR, level Q2) and without QIR. Consequently, the whole coronal lung data set of each study participant was used for comparison with coronal lung MR images acquired at 0.55 T field strength. CT window settings were constant at all images (center: - 500, width: 1700), with represents the standard window setting at our institution [6].
MRI Protocols and Image Acquisition
All MR exams of the chest were performed at the same 0.55 T MR whole body scanner (MAGNETOM Free.Max, Siemens Healthineers, Erlangen Germany) with a maximum slew rate 40 T/m/s, a maximum gradient amplitude 25 mT/m and 80 cm bore size. Volumetric Interpolated Breath-hold Examination (VIBE) sequence parameters (TR 10 ms, TE 2,89 ms, slice thickness 3 mm, flip angle 17°, FoV 400 mm, FoV phase 81%, distance factor 20%, phase oversampling 5%, 92 slices in one 3D block were acquired in 17 of 20 SSc patients. Spiral VIBE (TR 8.80 ms, TE 0.05 ms, flip angle 6°, SD 2.08 mm, voxel 2.1x2.1x2.5 mm, FoV 100%, FoV 600 mm, distance factor 20%, 106 slices) was acquired in 3 of 20 SSc patients [7].
Quantitative and Qualitative Image Analysis and Interrater Variablity
Three radiologists each for pHRCT and separate radiologists for MRI were selected to assess SSc-ILD according to the following categories: interstitial fibrotic lesions (0=none, 1=focal, 2=several lung areas, 3=diffuse lung affection); ground glass opacities (NSIP) (0=none, not visible, 1=focal, 2=several lung areas, 3=diffuse lung affection); pleural nodules/thickening (0=none /not visible, 1=focal, 2=several lung areas, 3=diffuse lung affection); estimated ILD alterations of both lungs (0=none, 1=0-20%, 2=20-40%, 3=40- 60%, 4=60-100%)
All images to be analysed were blinded to name, age and gender for all investigating radiologists (three for pHRCT, three for MRI), and the radiologists had no knowledge of the pHRCT or MRI findings of the other radiologists.
Statistical Analysis
The correlation (according to Pearson and Spearman) between the pHRCT and MRI findings (n=60 corresponding to 3x20 findings respectively) was determined using SPSS version 29.0.1.1, a p-value<0.05 was assessed as significant. The interrater-investigator variability (between the three radiologists) was evaluated according to Fleiss kappa modality. Fleiss kappa lower than 0.2 was determined as poor concordance respectively high interrater variability, between 0.2 and 0.4 as intermediate and higher than 0.4 as moderate respectively acceptable interrater variability [8]. The differences between Fleiss kappa values of pHRCT and MRI were detected as follows: the differences of scores of imaging findings between the blinded raters were summarized for each category of evaluation, and the summarized values were tested for significant differences between pHRCT and MRI applying the t-test (for related samples).
Results and Discussion
The evaluations showed a relatively high agreement in the category’s interstitial fibrosis degree (Pearson correlation 0.829) and gradual expression of ILD quantitatively (0.753), lower for alveolitis and pleural thickening (Figure 1). The results in all four categories had in common that the MRI mostly underestimated the severity due to the evaluation matrix. The interrater variability was moderate (Fleiss kappa >0.4) between the three-radiologist evaluating the SSc-ILD in pHRCT for all categories except ground glass opacities (kappa: 0.306), whereas the interrater variability was significantly higher in MRI findings according to the scoring evaluation matrix compared to pHRCT: Fleiss kappa for MRI 0.05-0.256 vs. pHRCT 0.306-0.527, (Figure 2).
To the best of our knowledge, this is the first study to examine the findings of pHRCT compared to MRI in patients with SSc-ILD in a blinded design, quantifying and statistically analysing the differences. MRI appears to underestimate the findings compared to the previous standard of imaging with pHRCT. The differences were particularly impressive in the evaluation categories of ground glass capacities and the quantitative assessment in % of affected lung sections in SSc-ILD. Only in the categories of interstitial fibrotic lesions and pleural thickening/nodules were the agreement values>50% (but always below 75%). In combination with the separate evaluation of interrater variability according to pHRCT and MRI, it can be seen that MRI not only underestimates the radiological findings of SSc-ILD, but that MRI findings are evaluated differently. In particular, ground glass opacities or the percentage extent of SSc-ILD in the lung appear to be difficult and inconsistent to assess.
There are no comparative studies on SSc-ILD in the literature. For interstitial lung disease of non-rheumatologic entity there are studies which detect inter-reader variability and relatively low inter-modality concordance, in detail, for assessment of pulmonary groundglass and fibrosis-like opacities [9]. However, in the clarification of tumor-suspicious lung lesions or pulmonary embolism, the CT scan appears to have better detectability than the MRI with VIBE sequence, especially the smaller the lesions are [10,11]. MRI of the lung in SSc-ILD should therefore be performed in selected centres with sufficient experience in the diagnosis, otherwise underestimation of SSc-ILD cannot be ruled out, with potentially negative consequences for treatment planning and prognosis. The results presented suggest that pHRCT is still superior to MRI, but that there is great potential for MRI by further improving the technology and adapting the software - especially in the assessment of interstitial fibrotic lesions. In the future, the supportive evaluation of MRI can be improved by AI and possibly also correlated with certain lung function parameters such as forced vital capacity - a marker that plays a decisive role in determining the prognosis of SSc-ILD.
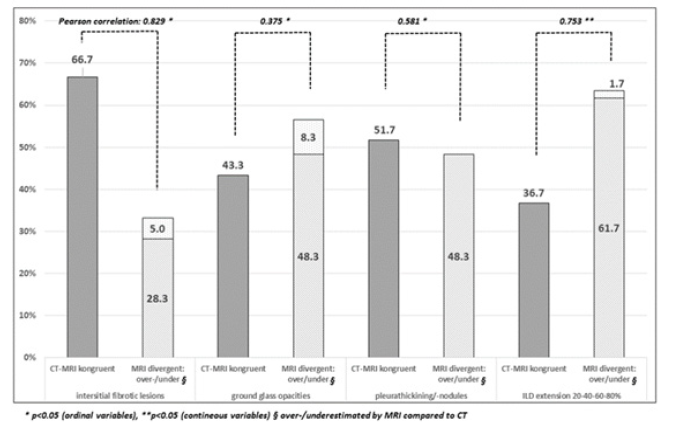
Figure 1: Comparing SSc-ILD imaging by HRCT and MRI in correlation in %values according to evaluation matrix and under-/overestimating pathological findings by MRI.
Note*: CT=photonen counting high resolution computed tomography; MRI= magnetic resonance imaging; ILD=interstitial lung disease.
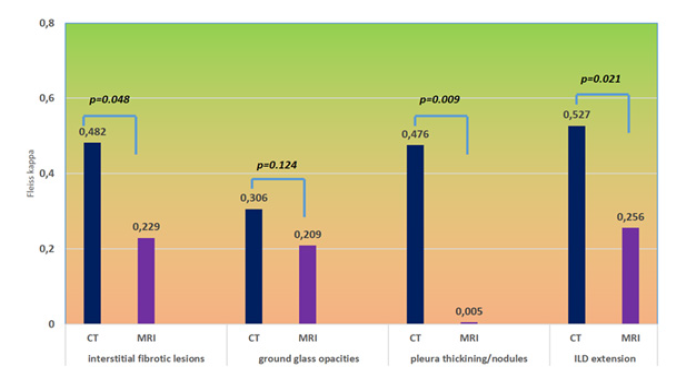
Figure 2: Interrater variability for different categories in imaging of SSc-ILD with pHRCT and MRI measured by statistical evaluation of Fleiss kappa, respectively
Note*: CT=photonen counting high resolution computed tomography; MRI= magnetic resonance imaging; ILD=interstitial lung disease.
Conclusion
The study shows acceptable correlation of the pHRCT findings with the MRI findings, particularly with regard to the degree of fibrosis in SSc-ILD, although the MRI findings have been significantly underestimated in comparison with HRCT. Furthermore, the interrater variability of radiologist were significant higher in MRI than in pHRCT findings. In our opinion, it is essential to specify the evaluation software for MRI optimizing the imaging of the special features of the lung parenchyma; further prospective studies to improve the MRI modalities are recommended before a broader use of MRI in SSc-ILD might be proposed.
Disclosure of Interest
Gunter Assmann Boehringer Inglheim, UCB, AbbVie, Vifor Pharma, Astrazeneca, Novartis, Turkiewicz Ryszard MSD, BMS, Boehringer-Inglheim, Janssen, Muecke Ramona, Gellrich Finn Markus, Shahzadi Iram, Niehoff Julius, Borgrefe Jan, Moenninghoff Christoph, Michael Schmidt: none declared.
Acknowledgement
None.
References
- Hunzelmann N, E Genth, T Krieg, W Lehmacher, I Melchers, et al. (2008) The registry of the German Network for Systemic Scleroderma: frequency of disease subsets and patterns of organ involvement. Rheumatology 47(8): 1185-1192.
- Nihtyanova SI, Benjamin E Schreiber, Voon H Ong, Daniel Rosenberg, Pia Moinzadeh, et al. (2014) Prediction of pulmonary complications and long-term survival in systemic sclerosis. Arthritis Rheumatol 66(6): 1625-1635.
- Woeltjen MM, JH Niehoff, Arwed Elias Michael, Sebastian Horstmeier, Christoph Moenninghoff, et al. (2022) Low-Dose High-Resolution Photon-Counting CT of the Lung: Radiation Dose and Imaging Quality in the Clinical Routine. Diagnostics 12(6): 1441.
- Masaaki Hori, Akifumi Hagiwara, Masami Goto, Akihiko Wada, Shigeki Aoki (2021) Low-Field Magnetic Resonance Imaging: Its History and Renaissance. Invest Radiol 56(11): 669-679.
- Kowal Bielecka O, Fransen J, Avouac J, Becker M, Kulak A, et al. (2016) EUSTAR Coauthors Update of EULAR recommendations for the treatment of systemic sclerosis. Ann Rheum Dis 76(8): 1327-1339.
- Sartoretti T, Racine D, Mergen V, Lisa Jungblut, Pascal Monnin, et al. (2022) Quantum iterative reconstruction for low-dose ultra-high-resolution photon-counting detector CT of the lung. Diagnostics 12(2): 522.
- Juergen Biederer (2023) MR imaging of the airways. Br J Radiol 96(1146): 20220630.
- Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1): 159-174.
- Lea Azour, Rany Condos, Mahesh B Keerthivasan, Mary Bruno, Terlika Pandit Sood, et al. (2022) Low-field 0.55 T MRI for assessment of pulmonary groundglass and fibrosis-like opacities: Inter-reader and inter-modality concordance. Eur J Radiol 156: 110515.
- Olthof SC, Reinert C, Nikolaou K, Pfannenberg C, Gatidis S, et al. (2021) Detection of lung lesions in breath-hold VIBE and free-breathing Spiral VIBE MRI compared to CT. Insights Imaging 12(1): 175.
- Ohno Y, Koyama H, Yoshikawa T, Seki S, Takenaka D, et al. (2016) Pulmonary high-resolution ultrashort TE MR imaging: Comparison with thin-section standard- and low-dose computed tomography for the assessment of pulmonary parenchyma diseases. J Magn Reson Imaging 43(2): 512-532.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.